Wednesday, August 09, 2017
Five-year SPNS initiative results presented at HRSA meeting
On June 27, 2017, the grant recipients of the Special Projects of National Significance (SPNS) funded initiative Building a Medical Home for Multiply Diagnosed HIV-Positive Homeless Populations convened a day-long meeting to present results to staff from the U.S. Department of Housing and Urban Development (HUD), Health Resources & Services Administration (HRSA), and Substance Abuse and Mental Health Services Administration (SAMHSA). They presented the strategies that collectively led to more than 1,300 people nationwide being served over the five-year initiative. The initiative focused on a group of people living with HIV who faced multiple barriers to accessing care and adhering to treatment: those who are experiencing homelessness and are diagnosed with substance use or mental health disorders. The Center for Advancing Health Policy and Practice (CAHPP) partnered with Boston Health Care for the Homeless to serve as the Evaluation and Technical Assistance Center for the project, known as Med-HEART (Medical Home-HIV Evaluation & Resource Team).
 The goals of this meeting were to inform development of strategies for providing care, share successes and challenges for achieving integrated care and housing stability, and identify opportunities for policy reform to improve services, all focused on people who are living with HIV, experiencing homelessness, and diagnosed with mental health or substance use disorders.
The goals of this meeting were to inform development of strategies for providing care, share successes and challenges for achieving integrated care and housing stability, and identify opportunities for policy reform to improve services, all focused on people who are living with HIV, experiencing homelessness, and diagnosed with mental health or substance use disorders.
As people entered the meeting room, they had the opportunity to view poster presentations outlining the model that was developed at each of the nine SPNS demonstration sites. The posters included findings, successes, challenges and next steps for each site. As they made their way to their seats, attendees also picked up one-page handouts providing an overview of each site’s model of care.
Introductions

From left: Harold Phillips, Melinda Tinsley, Serena Rajabiun, and Laura Cheever discuss last-minute details as attendees take their seats.
Harold Phillips, director, Office of HIV/AIDS Training and Capacity Development, HRSA, kicked off the meeting by outlining the meeting goals and emphasizing the focus on innovative models of care for people who are living with HIV, experiencing homelessness, and diagnosed with mental health or substance use disorders. “It’s really about improving service delivery and designing better ways to engage people in care, keeping them there, and getting them virally suppressed,” said Phillips.
Dr. Laura W. Cheever, associate administrator of the HIV/AIDS Bureau, HRSA, set the context of the initiative within the framework of broader efforts in the Ryan White program. “We have significantly improved viral suppression from about 69% to 83% among people in care,” Cheever said. “But that is for people who walk through the door at least once a year. We are desperately interested in the 400,000 people that aren’t in care, who aren’t virally suppressed. We have huge gaps in our knowledge about who those people are and how to reach them. This project is filling a gap we have in terms of an evidence base about what it takes to reach people with risk factors related to mental health, substance use, and being unstably housed.”
Overview of the SPNS Program and the Initiative
According to Dr. Cheever, the initiative was the “brain child” of Melinda Tinsley, SPNS public health analyst and the initiative’s project officer, who crafted a project that explored how to engage with people living with HIV who have co-occurring challenges of mental health, substance use and homelessness. Adan Cajina, branch chief of the SPNS program, gave an overview of the program.
The initiative is part of the Special Projects of National Significance (SPNS) program. SPNS initiatives are charged with the development of innovative models of HIV treatment, in order to quickly respond to emerging needs of clients served by Ryan White HIV/AIDS Programs. “I have never seen an initiative that has been so successful—you hold the record of most enrollees in a SPNS initiative,” said Cajina. “The retention among this population has been one of the best I have ever seen. This is what HRSA is all about—understanding how we improve the quality of care and improve the health outcomes of disenfranchised populations in the U.S. who are living with HIV/AIDS. Your legacy will live on in the publications that will come out in the next 6-8 months.”
Overview of Demonstration Models and Outcomes
Serena Rajabiun from Boston University, principal investigator of the evaluation and technical assistance center for the initiative, gave a brief overview of the program model used at nine sites nationwide. The intervention consisted of mobile navigators working intensely one-on-one with clients to determine each individual’s care needs and overcome barriers to receiving services. The navigators linked clients with a multidisciplinary and coordinated care team that included HIV care, substance use, mental health, and housing service providers. Length of intervention time was generally about 18 months, and navigators’ active caseloads averaged about 20 to 30 clients.
The 1,332 clients served were people 18 years of age or older who were living with HIV/AIDS, experiencing homelessness or unstable housing, and were diagnosed with co-occurring mental health and/or substance use disorders. Of the 909 individuals who participated in a multisite study associated with the intervention, upon enrollment many faced multiple barriers to care: 81% had a history of incarceration, 75% were diagnosed with a mental health condition, 24% were high risk for substance use dependency, 78% reported regular substance use, more than half said they experienced HIV stigma, and 59% had experienced food insecurity within the past 30 days.
Results of the study are promising: There were significant reductions in unmet needs and barriers to care. The number of clients who were unstably housed dropped from 84% to 36% over 18 months. Of the clients who were out of care or newly diagnosed at initial enrollment (N=334), 84% were linked to care; 74% were retained in care, and 71% achieved viral suppression by 12 months.
Maurice Evans, navigator team lead at Multnomah County HIV Health Services Center in Portland, OR, spoke about the project from the navigator and client perspectives. “Even though we were doing the same work, each site had to approach it differently because of where we were; we had to learn to navigate the system in our local areas and figure out how can we pull resources together to serve those clients who are on the bottom rung,” explained Evans. “We looked at the social determinants of health, including the most important one: the basic need to love and be loved. We were faced with this challenge to find out what people’s greatest needs were, and in the process of removing barriers, we were able to form bonds and relationships with them, and they trusted us. Because we were leading them to where they wanted to go, not where we wanted them to go. We took that time to really engage the people we were working with; we valued them as human beings.”
To highlight the impact of the relationship between navigator and clients, a video was shown showcasing clients from several locations talking about the impact of the SPNS project on their lives:
(More videos from several of the SPNS projects are available on our client story videos page.)
Panel: Transforming the medical home model to engage and retain PLWHA who are diagnosed with a mental health or substance use disorder and are homeless/unstably housed

From left: Ruthanne Marcus, Yale University, New Haven, CT; Lisa McKeithan, CommWell Health, Dunn, NC; and Kristin Barret and Kendall Guthrie, UF CARES, Jacksonville, FL, presented the medical home models their teams created as part of the initiative.
In a panel moderated by Carole Hohl and Sandy Sheble-Hall from Boston Health Care for the Homeless, representatives from three sites presented the medical home models they created to engage clients in care. Kendall Guthrie, program director, introduced the PATH Home project in Jacksonville, FL, which located the medical home model within a behavioral health and housing program. PATH Home is a collaborative partnership in which University of Florida Center for HIV/AIDS Research, Education and Service (UF CARES) integrated its HIV care providers into two half-day clinics per month within River Region Human Services, one of the area’s largest providers of housing, mental health and substance use services. The model included intensive case management and peer navigation for 167 clients, 47% of whom have now transitioned to standard of care.
View the PATH Home poster presentation
Lisa McKeithan, principal investigator and project manager for the NC-REACH project at CommWell Health in Dunn, NC, introduced the model at the only rural site in the initiative. NC-REACH integrated its Positive Life framework for HIV treatment with a comprehensive care coordination team. Patient navigators and care coordinators provided tailored services to help clients overcome barriers as they accessed housing, behavioral health, substance use treatment and HIV primary care services. One major challenge, McKeithan noted, was the lack of public transportation. “We don’t have taxis, we don’t have the metro, we don’t have subways—it’s our network navigators who are providing the transportation. Sometimes they would go 60 to 90 miles to pick up our patients to bring them into care.”
A major success of the program was the creation of a community housing coalition in which service providers—homeless shelters, substance use centers, incarceration centers, HOPWA, private landlords and more–come together to share information about their programs and resources. What began as a one-time meeting has continued as a once-per-quarter meeting that helps to build community systems and enhance housing opportunities for patients that will continue beyond the end of the SPNS initiative.
View NC-REACH poster presentation
Ruthanne Marcus, program manager for the mHEALTH project at Yale University in New Haven, CT calls the mHEALTH project “a patient-centered medical home without brick and mortar, providing care to people where they are.” A mobile medical home in the form of Yale’s big blue bus served as the hub, providing a wide range of services, including medical case management, primary care, and behavioral health services, to clients. The coordinated system of care included partners at Liberty Community Services, who provided housing services, and behavioral health services. Behavioral health services were provided by a psychiatric nurse practitioner and a social worker. Van services were extended by a centrally located “storefront” that provided a range of medical and drug treatment programs. A key component of the project was the collaboration with the Connecticut Department of Correction, which referred people who were being released from prison to the mHEALTH program.
View Project mHEALTH poster presentation
Panel: Integrating and sustaining care for PLWHA who are diagnosed with a mental health or substance use disorder and are homeless/unstably housed

From left: Angelica Palmeros, Pasadena Public Health Department, Pasadena, CA; Nancy Miertschin, Harris Health Systems, Houston, TX; and Manisha Maskay, Prism Health North Texas, Dallas, TX; participated in a panel to discuss how to integrate and sustain care for people living with HIV who are experiencing homelessness.
The purpose of this panel, according to Rajabiun, who served as moderator, was to gain a better understanding of how different projects integrated and sustained care for the population of focus. “We hope to share some tips in how to keep these programs going, so other organizations around the country can replicate some of the work they are doing,” Rajabiun said.
Manisha Maskay, chief program officer at Prism Health North Texas in Dallas, TX, said the Health Hope and Recovery (HHR) project, for which she served as principal investigator, filled a gap for the community they serve—in 2015, more than 50% of Prism Health’s clients living with HIV screened positive for substance use and mental health disorders and 6% were experiencing homelessness. The HHR model is an extremely client-centered, intensive care coordination and behavioral health intervention that utilized three full-time social workers who were knowledgeable about the treatment of HIV as well as mental health and substance use disorders, familiar with necessary community resources, and skilled in providing care to people with complex needs. “And they are mobile,” said Maskay. “They went where they’re needed, under bridges sometimes. They were effective at advocating for clients with housing, behavioral health, and medical providers.”
One strategy that proved very successful was to build relationships with rental property managers and owners; this served not only to get people housed, but to help them stay housed. The emergency housing agreements with hotels that were set up as part of the initiative also helped with the transition to stable housing. “You can’t just put a person who has been homeless for many years into a home and expect them to be OK with it. Having a hotel available for about 4 weeks with consistent guidance and help from the care coordinators was really important,” explained Maskay. Other important strategies included rigorous evaluation to understand which activities were most effective, enhancing the transition process to standard of care by training a specialized case management team that knew about helping people to get housed, constant active participation in partnerships, and subscribing to the Housing Management Information System to expedite clients’ access to permanent housing.
View Health, Hope and Recovery poster presentation
Nancy Miertschin, HIV project manager at Harris Health, introduced the Hi-5 project in Houston, TX. Hi-5 was a trauma-informed intensive case-management program that focused on prioritizing client’s primary needs for housing, HIV care, and mental health and substance use treatment. Within Harris Health System’s large network that includes three hospitals and 26 community centers, the HIV clinic is located at the Thomas Street Health Center, serving over 6,000 patients, including half of Harris County’s uninsured HIV patients. About 1,000 of the clinic’s HIV patients were experiencing homelessness or unstable housing. The HIV clinic partnered closely with Harris Health’s Health Care for the Homeless program. “In the beginning we didn’t speak each others’ languages,” said Miertschin. “A big part of our project has been for the HIV staff to train homeless care givers, and we, on the HIV side, have learned a lot about reaching out and retaining patients experiencing homelessness in care.”
Three medical case managers, who were licensed masters-level social workers, and two service linkage workers provided case management services for Hi-5. Staff began planning for sustainability 2 to 3 years before the end of the SPNS project, Miertschin explained. Service linkage workers were trained to be certified to provide every function in their extensive job description, including rapid HIV testing, to increase flexibility in the way they were deployed. A policy at Thomas Street uses the highest standard of care definition so that services are in compliance with standards for various funding sources, such as Ryan White Part A. The Hi-5 team also leveraged training for existing HIV case management staff at Thomas Street so that Hi-5 linkage workers were included in all trainings and participated in regular combined meetings and shared supervision. Miertschin provided a monthly report on the Hi-5 project to the Ryan White Planning Council. She closed her presentation with some “breaking news”: As a result of the promising results of the Hi-5 project, the Ryan White Planning Council’s allocation process has decided to provide four case management positions dedicated to serving people experiencing homelessness.
View Hi-5 poster presentation
Angelica Palmeros, division manager, Social and Health Programs, Pasadena Public Health Department (PPHD) and principal investigator for the Operation Link project, characterized her health department as a small, gray dot within the much larger area of the Los Angeles basin, which has the largest homeless population in the country. As they were implementing their project, the PPHD went through a transformation: because of changes in the health care landscape brought about by the Affordable Care Act, the PPHD transferred all clinical services to the John Wesley Health Center, a local federally qualified health center. “Luckily, we have fantastic peer navigators who knew how to handle all the stress,” said Palmeros. “The fact that the clients were connected with the peer navigators helped to keep them calm. We had to look at sustainability with a whole different lens because now everything about our organization had changed.”
Elements that will continue beyond the end of the project include the training and education providers received in working with the Operation Link team and clients. In addition to providing training on the needs of people experiencing homelessness, the team did a lot of work around cultural sensitivity and improved understanding of the needs of the LGBT and transgender community.
With the SPNS project coming to a close, the team is now focused on “Operation Link 2.0” which will expand to provide services to individuals not living with HIV but facing other challenges associated with other chronic diseases, homelessness, or health disparities. Based on the success of the Operation Link model, the Pasadena Public library has received a grant to sustain a peer care navigator position in the Pasadena library system to reach out to people experiencing homelessness and link them to services. A proposal requesting funding for a second navigator in the library system is also in the works. In partnership with the Pasadena Police Department, the PPHD was also awarded a two million dollar grant to provide reentry services in a peer navigator model to support people facing mental health and substance use disorders and help them address housing and other needs. “A lot of times, people experiencing homelessness are dehumanized,” said Palmeros. “This project gave us an opportunity to recognize the clients and enable them to be part of the process. “
View Operation Link poster presentation
Panel: Building relationships that connect PLWHA who are diagnosed with a mental health or substance use disorder and are homeless/unstably housed with needed services

Clients and the providers who worked with them shared their experiences: From left, Deb Borne, Scott Carlisle, San Francisco Department of Public Health, SF, CA; Myranda Harris, Jamie Christianson, Multnomah County Health Department, Portland, OR; and Michael Delaney and Amelia Broadnax, Family Health Centers of San Diego, San Diego, CA
For many, the highlight of the day was hearing directly from the people whose lives were affected by the initiative. In this panel discussion moderated by James Apt from Boston Health Care for the Homeless, three clients shared the stories of how they worked with their medical teams to find and maintain stable housing, reconnect with HIV care, and address mental health and substance use disorders. As Myranda Harris described it, “So many things in my life have been restored—my mind, my emotions, the relationship with my daughter. I’m really grateful.” Learn more about the stories behind the numbers, as demonstrated by the experiences of these three individuals.
View poster presentations from the three sites represented in this panel:
Summary of findings, policy implications & opportunities for Ryan White Parts & other federal resources
Links to program resources can be found on the Med-HEART project page.
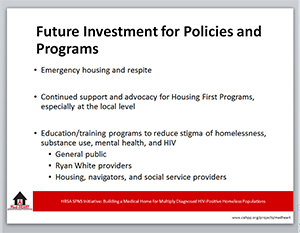
Rajabiun wrapped up the meeting with a summary of project results and recommendations. Key components included mobile care, integrated services that incorporate HIV primary care, substance use and mental health treatment, housing and social services, and a trauma-informed culture that welcomes people living with HIV and experiencing homelessness. Intensive and ongoing training for staff and support for the navigators on the front line of building trust and working with clients to eliminate barriers to care was also crucial. “Clothing, food, showers, hygiene packages, access to cell phones, documentation so people can access the services they need–we need to address basic needs and the social determinants of health,” said Rajabiun. “We just saw Anthony Fauci [director of the National Institute of Allergy and Infectious Diseases] talk at BU. He said we can have the best medical interventions, but if we don’t address those social needs, we’re not going to get anywhere in improving health outcomes. This project showed what we need to do to get there. Mobile, integrated, intensive care—that’s how you reach people who are homeless, multiply diagnosed and living with HIV.”
More information about the initiative can be found on the Med-HEART project page.