|
|
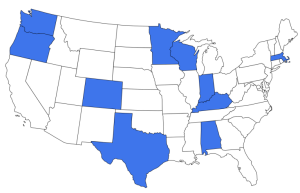
The federal Maternal and Child Health Bureau has funded this 10-state Collaborative Improvement and Innovation Network (CoIIN) to test and spread promising care delivery strategies and payment models for children with medical complexity (CMC). The three-fold goals of the project are to improve: 1.) The quality of life for CMC CMC have significant, chronic health problems that affect multiple organ systems, resulting in functional limitations, high health care need or utilization and often the need for or use of medical technology. Their care is typically fragmented, and their families often experience stress and financial hardship. Providers routinely encounter barriers to delivering high quality, value-based health care that supports the physical, emotional, mental and social well-being of CMC and their families. This document highlights the work that the Boston University leadership team and each of the 10 state teams have completed since the start of the project in 2017. |
Who we Are
|
10 state teams, 148+ team members, 2,290 CMC enrolled in interventions, 5 partner organizations, & a 20-member national advisory committee Team Members Represent:
Centering Family Partnership:
|
|
What We do & How
|
|
Technical Assistance Technical assistance by the Boston University leadership team and the collaborative partners to state teams included:
|
CMC & COVID-19 Extension for Community Healthcare Outcomes (ECHO)
A partnership with the American Academy of Pediatrics, this program leveraged tele-mentoring video conferencing technology to increase inter-professional participant knowledge, capacity, comfort and competence in caring for CMC during the COVID-19 pandemic.
- 212 participants, including CoIIN members and providers nationwide
- 28 ECHO sessions and topics
- 20 guest speakers
- 15 faculty
- 93.3% of participant responders were satisfied with the ECHO and found it a valuable use of their time
National Care Coordination Academy
This partnership between the CMC CoIIN and Boston Children’s Hospital:
- Engaged 5 state teams and 9 external teams in collaborative learning and peer mentoring
- Focused on 3 key themes
- Care coordination implementation
- Measurement of effectiveness
- Sustainability
- Provided ongoing technical assistance to member teams
|
Evaluation and Quality Improvement
|
|
Dissemination Products
- 96 products developed by the Network in the Implementation Library
- 60+ presentations to date by Boston University, partners, and state teams
- 10 articles and manuscripts
- 11 infographics
- 30+ graphic recordings
State Team Work
Here we highlight each state team’s main focus and one of their many accomplishments from this project.
While all CoIIN teams worked toward common network objectives, they each focused on individual projects specific to their state, service delivery system, and patient population.
Common threads among state teams’ individual projects included improving care coordination, creating Shared Plans of Care (SPoCs) with families, and ensuring all patients had access to a medical home.
Focus: Improving care coordination for CMC
Work Highlight: Provided families with a Care Notebook developed by Family Voices Alabama to establish parent-to-parent support and facilitate care coordination
Focus: Improving collaboration and communication between family, primary care, and subspecialty providers using a co-management approach
Work Highlight: Created a Role Clarification Tool within the electronic medical record system so that families can quickly access who to contact for each of their child’s needs
Focus: Creating a primary-tertiary care coordination collaborative to produce comprehensive, functional, and fluid SPoCs for CMC and their families
Work Highlight: Developed a comprehensive care coordination curriculum to train and mentor nurse coordinators
Focus: Utilizing teleconferencing technology for patient-centered care planning services and creating a comprehensive clinic for CMC recently discharged from the NICU
Work Highlight: Utilized existing Virtual Care Team Conference framework to quickly implement telehealth visits for CMC during the COVID-19 pandemic
Focus: Developing a Shared Surgical Plan of Care for children undergoing hip, spinal fusion, or baclofen pump surgery to identify pre-surgical medical needs
Work Highlight: Focused on family engagement to make the perioperative process smoother and safer for CMC and their caregivers
Focus: Partnering with families to implement family-centered SPoCs to move more care into the community and decrease acute episodes and hospitalizations
Work Highlight: Integrated paid parent advisors into the project team as equal partners for ongoing feedback and improvement
Focus: Preparing young adults with medical complexity to transition to adult care providers through the use of a SPoC and Health Passport
Work Highlight: Created a one-year, three-stage program to guide patients and families through the process of establishing adult primary care
Focus: Building a family-centered, integrated care delivery system that eliminates fragmentation, optimizes satisfaction, and improves health outcomes
Work Highlight: Developed a ‘Touchpoints’ graphic system to analyze time and effort spent on care tasks for individual patients
Focus: Helping families of infants with medical complexity who were recently discharged from the hospital build resiliency by engaging with public health, community, and medical resources
Work Highlight: Increased the percentage of families engaging with Early Intervention services by following up with families and providers
Focus: Improving the service delivery system for CMC through the development of care coordination tools and supporting enrollment of eligible CMC into the Children’s Long-Term Supports (CLTS) waiver program
Work Highlight: Developed a Goal Card tool to break down complex needs into achievable goals that are meaningful for the family
HRSA Statement
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number #UJ6MC32737: Health Care Delivery System Innovations for Children with Medical Complexity ($2,700,000 annually). This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsement be inferred, by HRSA, HHS or the U.S. government. Anna Maria Padlan, HRSA/MCHB Project Officer